In life it is rare to get everything at once. First, we strive to get education, then to achieve success in our professional field, then to create a family and give birth to our children. Each step takes time and energy. And these steps are so difficult to combine, for example, to achieve success at work while starting a family. And we, of course, want to do everything in the best possible way.
Equally, a successful and efficient IVF process requires a step-by-step and focused approach. For example, it may be not possible to create both competent embryos and receptive endometriumEndometrium — the lining covering the uterine cavity at the same time — each link in the reproductive chain may have its own individual rhythm, which we should hear, understand and accept, and only in this dialogue move towards the goal — pregnancy and live birth.
IVF is a big task and a big project both in terms of high expectations and huge emotional, physical and financial investments.
So that a big task does not look impossible, and a big project ungraspable, we divide it into separate stages. It allows us to focus on achieving the goals of each stage, and from these small goals get the main goal – an on-going pregnancy and live birth.
Below we describe our IVF process step by step. It will help you manage your expectations.
IVF process step by step. One challenge — one solution.
Each step of your IVF journey will have its own focus and goal:
| Steps in your IVF process and goals | Focus | Logistics |
| Month 1: IVF Cycle The Goal: Viable Embryo at BlastocystBlastocyst — the stage that a human embryo normally reaches on day 5-6 of development. This is the stage on which the embryo implantation begins. stage; normal for 23 chromosomeChromosome — is a unit of genetic information in a cell which contains DNA and proteins. Abnormal number of chromosomes in cells of embryos, makes an embryo’s development stop. An abnormal number of chromosomes in embryos, is responsible for 70-80% of pregnancy losses in the first 12 weeks pairs |
| Your ovarian stimulation takes place in your local country according to our Treatment Plan. You come to O.L.G.A. Fertility St. Peterbsurg/ Cyprus for 10 days — for laboratory tests, last ultrasound examinations and egg retrieval. Egg retrieval is planned day X+- 2 days. You can leave 24 h after. |
| Month 2: Cool Down Cycle The Goal: Cooling down ovaries after stimulation | Pill intake to help ovaries shrink after stimulation and stop producing residual levels of ProgesteroneProgesterone — the main pregnancy hormone. Progesterone production by the ovary begins at ovulation. Progesterone influences the endometrium and times its readiness for implantation — implantation window | |
| Month 3: HysteroscopyHysteroscopy — endoscopic check of uterus. “Hyster” = “Uterus” and “Scopy” = “Looking” in Greek. Hysteroscopy is done via the natural pathway. Hysteroscopy enables surgical treatment of problems inside the uterus which may be responsible for IVF failures Cycle The Goal: Diagnostics and possible microsurgical treatment of potential macroscopic findings in the uterine cavity; taking endometrial samples for cell/microbe/DNA/RNA tests; defining implantation windowImplantation window is a time frame under 72 hours when special receptors are present on the surface of endometrium, which can recognize receptors on the surface of embryos to start the implantation process Receptor — is a protein structure on the surface of one cell, which recognizes a specific molecule or another receptor on the surface of another cell (like a key and lock). With the help of receptors cells, they can communicate with each other. An example of such dialogue: implantation dialogue between embryonic cells and endometrial cells during the implantation process. |
| Your preparation for the Hysteroscopy and ERA test takes place in your local country according to our Treatment Plan. You come to O.L.G.A. Fertility St. Peterbsurg / Cyprus for 5 days — for laboratory tests, last ultrasound examinations, hysteroscopy, consultation, recommendations and prescriptions. |
| Month 4: After Hysteroscopy Treatment Cycle The Goal: Optimizing endometrium with the help of medication |
| |
| Month 5: Embryo Transfer Cycle The Goal: To achieve successful implantation and on-going pregnancy | Here all the three pieces of the puzzle should come together: transfer of a chromosomally normal blastocyst into your optimally prepared endometrium in the right timing | Your preparation for your Embryo Transfer takes place in your local country according to our Treatment Plan. You come to O.L.G.A. Fertility St. Peterbsurg/Cyprus for 5 days – for laboratory tests, last ultrasound examination, consultations with doctors and nurses, your Embryo Transfer, recommendations and prescriptions. |
| Potential months 6,7,8. More embryo transfers if necessary and possible The Goal: Potential next Embryo Transfer to achieve successful implantation and on-going pregnancy | In O.L.G.A. Fertility you have: 51.6% chance of live birth after 1 ET 75.4% chance of live birth after 2 ETs 85.6% chance of live birth after 3 ETs 88.9% chance of live birth after 4 ETs If after the first embryo transfer no pregnancy was achieved: a) In case there are chromosomally normal embryo(s) available after the last IVF cycle, the next embryo transfer can be done in the very next cycle. Important is that the patient does not stop hormonal medication before having spoken to the doctor. We usually book this call in advance for the doctor and the patient to speak as soon as the HCG test result is received. | |
| Your treatment after positive pregnancy test until Live Birth The Goal: A Baby |
|
Month 1
Your IVF Cycle
The Goal: to have a viable embryo at the blastocyst stage, normal for 23 chromosome pairs
We are often asked, if PGT-A improves egg and embryo quality?
No, PGT-A is only a method of embryo testing. It helps to eliminate good looking, but abnormal blastocysts from usage. It does not make your embryos better — it identifies those embryos with a normal set of chromosomes from those that are available.
To be able to test good looking embryos at blastocyst stage, we first need to create them. This may be challenging, especially in patients, who have not had any blastocysts in previous attempts. We learn from the past and know how to use this knowledge for the future success.
How to achieve viable blastocysts, even if past attempts have resulted in no blastocysts at all?
Step 1. Your Individualized stimulation
The Goal: competent eggs with sufficient levels of energy
Two women of the same age and the same AMH levels may benefit from different stimulation schemes. We gain knowledge and a good feeling based on your medical history, test results and information about your previous IVF attempts. When you thoroughly inform us of the data from your past IVF attempts, you create the basis for us to create a successful treatment plan for you.
During two weeks from the beginning of the cycle till ovulationovulation — when the egg Is released from the ovary (or egg retrieval) eggs need to multiply their energy resources hundreds of times. It is clear enough that energy is needed to create a viable embryo. A sperm does bring half of a genome, but only the egg possesses the power stations for the development of the embryo. They are called mitochondria, if a cell was a city, mitochondria would be this city’s power plants.
Individualized and balanced treatment plan helps eggs to collect enough energy for fertilization and embryonic development.
We also recommend diet, lifestyle adjustments, vitamins and supplements aimed at increasing egg energy levels.
Step 2. A Gentle, quick, and painless egg retrieval
The Goal: one follicleFollicle — a mature follicle is a 2 cm bubble containing a 0,1mm egg. Follicles are located in the ovary — one mature egg
We take great care in making the egg retrieval gentle, quick, and painless, this ensures that the egg retrieval day will be a good day for all our patients.
During egg retrieval, we focus on every single follicle and every single egg. If our patient would like to proceed towards egg retrieval having even just one single follicle, we will go for it and do our very best.
Step 3. First class process in our EmbryoLab
The Goal: Blastocysts, Normal for 23 Chromosome Pairs
- Elegant and soft IVF and ICSI procedures
- Careful and reliable blastocyst growing
- PGT-A (genetic testing of embryos to find the normal ones from those available)
Little embryos are like children or flowers: they need to be talked to in a nice way and handled with love and care. Our embryologists feel like they look after flowers or work in a kindergarten, rather than growing embryos :)
Dr. Svetlana Shlykova, Dr. Anna Gusareva and Dr. Maia Shestakova have hearts full of love and hands full of skill. The embryos in their lab gain all this special attention, love, and care.


Step 4. Gentle freezing of your blastocysts by vitrification (FREEZE ALL)
The Goal: to stop time for the embryos and use this time for optimizing your maternal side before embryo transfer
- Why don’t we transfer fresh embryos? — Because endometrial receptivity in stimulated cycles is lower than in natural cycles, or cycles on HRT.
- Why do we freeze all embryos? — We freeze all the embryos to stop time for them for a while so that we gain 1-2 months to focus on your endometrium and other maternal factors.
- Why not try with a fresh embryo right away and then try with a frozen embryo later, if fresh transfer hasn’t worked? — Because many patients will have just the one usable embryo and we must create VIP conditions for its transfer to achieve a maximum result.
- Why are we not afraid “to risk the embryo by freezing it”? — Because we have above 95% survival rates after freezing/thawing via vitrification.
 In many spheres of our life we cannot get two goals at once and chasing two rabbits at once will just lead to catching none.
In many spheres of our life we cannot get two goals at once and chasing two rabbits at once will just lead to catching none.
In many patients getting eggs and embryos is like one rabbit and preparing an optimal endometrium and implantation window like the other, and we can catch both only when we chase them one by one, in a separate setting and timing.
Logistics
Your ovarian stimulation takes place in your local country according to our Treatment Plan. You come to O.L.G.A. Fertility St. Peterbsurg/ Cyprus for 10 days — for laboratory tests, last ultrasound examinations and egg retrieval. Egg retrieval is planned day X+- 2 days. You can leave 24 h after.
Month 2
Cool Down Cycle
The Goal: to give ovaries time for cooling down after stimulation
Several weeks after stimulation, even after menstruation, ovaries may still be hormonally active, producing Estrogen, and especially Progesterone. Normally Progesterone is being produced only after ovulation and declines to zero by the time of menstruation. Production of Progesterone during and after menstruation makes endometrium not receptive in the current cycle. Therefore, usually the cycle after a stimulated cycle is used for giving ovaries rest. Ovaries need to cool down and shrink before beginning of the cycle in which the embryo transfer or ERA test (defining the implantation window) is planned. Pill intake from the start of menstruation, which comes within 2 weeks after egg retrieval, helps ovaries shrink after stimulation and stop producing residual levels of Progesterone. Usually after 3 weeks of pill a woman is ready to start the embryo transfer cycle or hysteroscopy/ERA test cycle.
Month 3
Hysteroscopy Cycle
The Goal: Diagnostics and possible microsurgical treatment of potential macroscopic findings in uterine cavity; taking endometrial samples for cell/microbe/DNA/RNA tests; defining implantation window
Hysteroscopy helps to find and micro-surgically treat macroscopic conditions which may negatively influence chances of implantation: polyps, micro polyps, adhesions etc.
Hysteroscopy may not be necessary for all patients. If hysteroscopy is not indicated, this cycle can be used for Embryo Transfer. Hormonal preparation for the embryo transfer and hysteroscopy is similar since the goal of Hysteroscopy in O.L.G.A. Fertility is to evaluate the place of implantation under the same conditions as for the actual embryo transfer.
Treatment in a Hysteroscopy cycle imitates an Embryo Transfer cуcle and consists of natural or synthetic Estradiol and Progesterone hormones; to imitate the phases of the normal menstrual cycle. If an ERA test is planned, a down-regulation injection is usually done several days before the beginning of the Hysteroscopy cycle to gain full control over hormonal levels and obtain reproducibility of the hormonal setting in the Embryo Transfer сycle.
We call this treatment a training cycle because this helps us evaluate your endometrial response to certain hormonal dosages in advance and choose the right hormonal dosage specifically for you in your Embryo Transfer cycle. Also, hormonal therapy with Estradiol and Progesterone helps to restore endometrial receptivity, even in those patients who have had impaired endometrial receptivity previously.
After we have had an opportunity of viewing your endometrium at different stages before and during stimulation and at the egg retrieval, we will come back to you with information as to whether we see any sonographic signs of polyps, adhesions, or other structures in endometrium, which may reduce the chances of implantation. If we see those potential reasons for a future failure, we will recommend a Hysteroscopy.
A Hysteroscopy is an endoscopic investigation of the uterine cavity — looking at the uterus from inside!
‘Hysteroscopy’ comes from the Greek meaning: “Hyster” = “Uterus” and “Scopy” = “Looking”.
Hysteroscopy provides us with the opportunity to look inside your uterus via a natural pathway, with the help of a tiny video camera. In O.L.G.A. Fertility, we do full surgical hysteroscopy under general anesthesia, which means we have the opportunity to infuse liquid in the uterus to straighten all the little corners of uterine cavity so as to see all the hidden details which may not be seen by quick office-based hysteroscopy. During a hysteroscopy we can treat possible abnormal findings (polyps, adhesions) microsurgically and hence increase the chances for a successful implantation.

Picture 1. Scratching, which is a nice “peeling for the endometrium” — lining of the uterus.
During a hysteroscopy, a scratching – like a peeling - might be performed to make the uterine cavity fresher, smoother, with better blood flow and more attractive for the embryo to implant.
During hysteroscopy several tissue tests are taken:
- Histological and immunohistochemical testing of the endometrium tissue helps to identify potential abnormalities at microscopic cell levels.
- PCR testing of the endometrium for bacteria and viruses.
- ERA test checks implantation window based on certain protein RNA expression levels in the endometrium.
ERA is an abbreviation for “Endometrial Receptivity Array”. The aim of the ERA test is to confirm on which day and time, after the start of Progesterone supplementation, the endometrium is most receptive to the embryo. In the majority of women, the implantation window takes place around day 6 of Progesterone supplementation and lasts around 60 hours. However, in 20-30% of women the implantation window may start earlier or later or last less hours. We believe it to be important to investigate the implantation window in patients who come to us after multiple unsuccessful attempts.

Picture 2. A metaphor for some of the causes of failure — findings in the uterus that make implantation difficult.
During a hysteroscopy, the reasons why it was hard for the embryos to implant in the past can be found: polyps, adhesions, inflammation and many others. Eliminating or correcting these intrauterine reasons of failure increases the likelihood of a future successful implantation and carrying pregnancy to term.

Picture 3. A VIP site for a VIP embryo to implant
Picture 3 is a metaphor for a well-prepared uterine cavity ready for embryo recognition and acceptance. After a hysteroscopy, removal of polyps or scar tissue, scratching, hormonal, immune and blood thinning therapy, it will be easier for the embryo to implant. It often happens that out of several blastocysts obtained within an IVF cycle, only one has a normal set of chromosomes. This is our VIP embryo, and our task is to create all the necessary conditions for its successful implantation.
Logistics
Your preparation for the Hysteroscopy and ERA test takes place in your local country according to our Treatment Plan. You come to O.L.G.A. Fertility St. Peterbsurg / Cyprus for 5 days — for laboratory tests, last ultrasound examinations, hysteroscopy, consultation, recommendations and prescriptions.
Month 4
After Hysteroscopy Treatment Cycle
The Goal: Optimizing endometrium with the help of medication
Within 2 weeks after Hysteroscopy, we receive results of histological, immunohistochemical and PCR testing of endometrium tissue.
Depending on the findings and micro-surgical treatment during hysteroscopy, specific treatment may be recommended: growth factors after having removed scar tissue and for thin atrophic endometrium, antibiotics, and antiviral medicines for chronic inflammation, immune therapy for signs of autoimmune aggression. The aim of this treatment is to optimize endometrium and increase chances of implantation in the future.
In some cases, such as with endometriosis, we may recommend longer treatments after hysteroscopy to suppress the endometriosis and its negative influence on implantation.
All the medication which needs to be taken after hysteroscopy and up until the embryo transfer, can be bought in our neighboring pharmacy, if necessary.
3 weeks after Hysteroscopy the result of the ERA test arrives, which provides information about how many hours after the start of Progesterone supplementation we should do the embryo transfer in the following cycle. Then we adjust the Treatment Plan accordingly.
At the end of this Month 4 (After Hysteroscopy Treatment Cycle) a down-regulation injection is usually administered to switch off ovarian hormone production for one month. The aim of this downregulation injection is to avoid premature ovulation. Premature ovulation may make the timing of your implantation window different from the one found optimal for your embryo transfer. This downregulation injection is also necessary for being able to accurately reproduce the implantation window in the Embryo Transfer Cycle.
The duration of downregulation treatment, without estrogen coverage in the hormonal scheme aimed at the embryo transfer, does not exceed 7 days, so the undesired symptoms are highly unlikely to appear in such a short period of time.
Month 5
Embryo Transfer Cycle
The Goal: To achieve successful implantation and on-going pregnancy
Here all the three pieces of the puzzle should come together: transfer of a chromosomally normal blastocyst into your optimally prepared endometrium in the right timing.
Medication to grow a receptive endometrium
After you have stopped Estradiol and Progesterone in your After Hysteroscopy Treatment Cycle or, if there was no hysteroscopy, then at the end of your Cool Down Cycle, menstruation begins, and this is the start of your Embryo Transfer Cycle.
As we know from the IVF Success chapter, the endometrium grows due to the Estrogens, which are prescribed in the Embryo Transfer Cycle in the form of tablets, patches and/or gels. We monitor the growth of the endometrium with the help of the ultrasound to assess the thickness and decide if additional doses of Estrogen are required.
The doses of Estrogens during the preparation for the embryo transfer are much lower than the levels of Estrogen during pregnancy, which are produced by the placenta.
For the patients who have previously faced the problem of thin endometrium, growth factors can be used to stimulate the growth of the endometrium, low molecular weight heparins — to improve blood flow. For the patients with the signs of immune system aggression — prednisolone, intralipids, and/or IVIG therapy may be used to make the woman's immune system friendly towards the embryo. After a thorough review of the previous attempts and your investigation in O.L.G.A. Fertility, the necessary medications are added to the Treatment Plan on an individual basis.
Progesterone
Progesterone intake usually starts six days before the embryo transfer date. If the ERA test showed that the implantation window is earlier or later, we adjust the start of the Progesterone accordingly.
We recommend taking two forms of Progesterone at once: vaginal suppositories / vaginal cream + injections. Why both? — This combination is the best way to reduce the incidence of bleeding, early pregnancy loss and increase the chances for an on-going pregnancy.
The Embryo Transfer itself
Our standard practice is a Single Elective Embryo transfer.
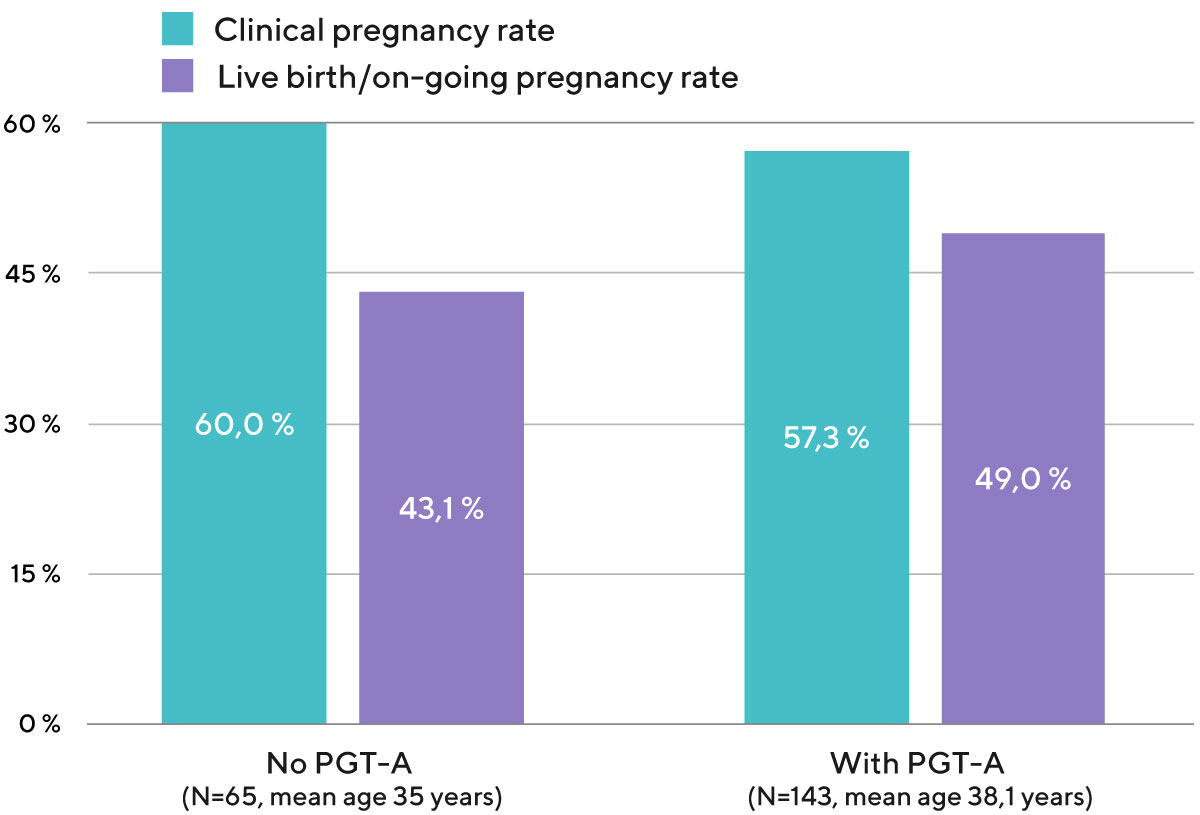
Out of 100 transfers of a single embryo with a normal number of chromosomes in O.L.G.A. Fertility, 51 end in a live birth. It means that each transfer of an embryo with a normal set of chromosomes in O.L.G.A. has a 51% chance of resulting in an on-going pregnancy and live birth (Diagram 1).
Diagram 1. Clinical pregnancy rate and live birth/on-going pregnancy rate per one embryo transfer with own eggs, depending on whether or not PGT-A was used to check the chromosomal status of the embryo (data from the embryo transfers performed in 2020 and 2021).
What is the chance of reaching an on-going pregnancy and live birth after the 2nd, 3rd and 4th embryo transfers in O.L.G.A. Fertility? (Diagram 2)
In O.L.G.A. Fertility you have:
- 51.6% chance of live birth after 1 ET
- 75.4% chance of live birth after 2 ETs
- 85.6% chance of live birth after 3 ETs
- 88.9% chance of live birth after 4 ETs
Diagram 2. Cumulative live birth rateLive birth rate — are calculated per embryo transfer. Live birth rates show percentage of embryo transfers which resulted in live birth in all groups of patients who received embryo transfers within 1131 consecutive embryo transfers at O.L.G.A. Fertility in the years 2019 — 2021)
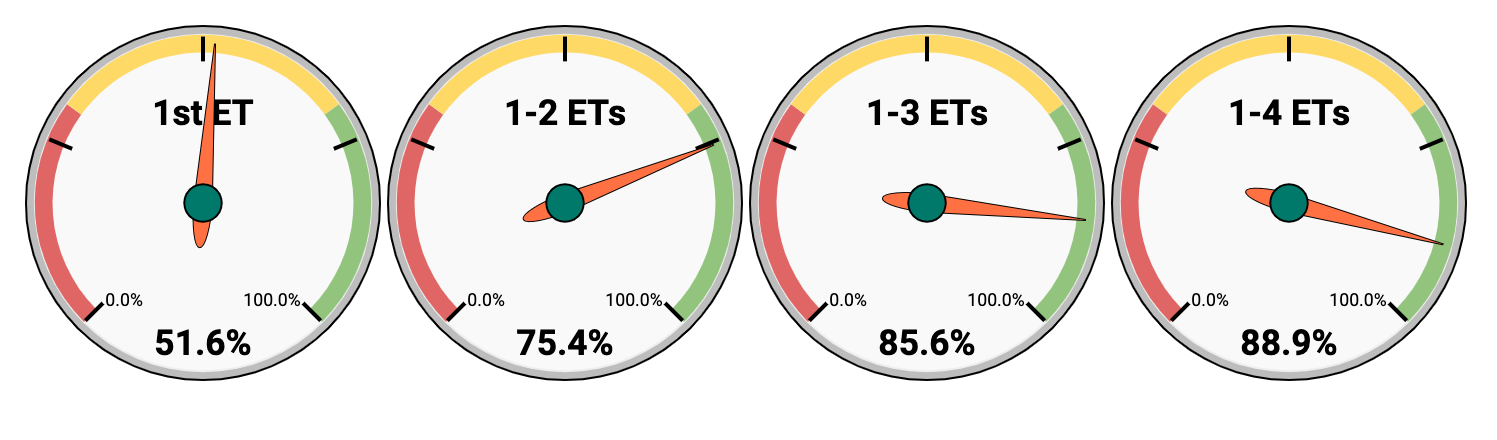
As a result, if we persevere and consistently move towards the goal, the chance of having a baby after 4 embryo transfers in O.L.G.A. Fertility is 88.9%.
When working with donor eggs, it will be quite easy to have 4 embryo transfers, because the donor has many eggs. Also, when we use donor eggs, blastocysts develop more frequently and most of them carry normal number of chromosomes.
When working with patients’ own eggs, especially in women after multiple IVF failures (to whom this entire page is devoted), the first challenging task is to obtain this golden VIP embryo — a morphologically usable blastocyst with a normal number of chromosomes. The second complex task is to create such VIP conditions in the uterus for this VIP embryo, so that the embryo couldn’t but agree to the offer made 😊 and implant with all the possible chances.
The transfer of two embryos will not increase pregnancy rates considerably but will significantly increase the life/health risks for the mother and the children if a twin pregnancy occurs. That is why we stick to the concept of preserving our high success rates, not through increasing the number of transferred embryos, but through clinical strategy and laboratory excellence.
Your Embryo transfer day is a very important day. All the recommendations about medication and further process are done by our doctors and nurses the day before so that on your embryo transfer day you are feeling confident and comfortable that all the steps following the embryo transfer are secured. We prepare for your embryo transfer to be a soft, gentle procedure and a happy experience for you.
Logistics
Your preparation for your Embryo Transfer takes place in your local country according to our Treatment Plan. You come to O.L.G.A. Fertility St. Peterbsurg/Cyprus for 5 days – for laboratory tests, last ultrasound examination, consultations with doctors and nurses, actual Embryo Transfer, recommendations and prescriptions.
Have questions?
Potential months 6, 7 or 8
More embryo transfers if necessary and possible
The Goal: Potential next Embryo Transfer to achieve successful implantation and on-going pregnancy
If after the first embryo transfer no pregnancy was achieved:
- In case there are chromosomally normal embryo(s) available after the last IVF cycle, the next embryo transfer can be done in the very next cycle. Important is that the patient does not stop hormonal medication before having spoken to the doctor. We usually book this call in advance for the doctor and the patient to speak as soon as the HCG test result is received.
- If there are no chromosomally normal embryos available, stimulation of ovaries can be started right away or after a short course of pill, based on medical/social/emotional situation.
- In some cases there may be a transition to using donor eggs based on medical situation, recommendation of the Clinic and patient’s decision.
Your treatment after positive pregnancy test until Live Birth
The Goal: A Baby
Once your embryo has been transferred into your uterus you will continue to take Estradiol and Progesterone for 10 days before taking a pregnancy test (this will be a blood test). Should the test result be positive, you will carry out an ultrasound scan 3 weeks later to confirm your pregnancy.
You will continue with your hormonal medication until 12-13 weeks of pregnancy when the placenta becomes mature and produces enough hormones to support the pregnancy itself. From this stage of pregnancy, you will not usually need more specific support than you would need in a naturally conceived pregnancy and the prognosis of carrying it to the full term is very good. After most of your hormonal support is discontinued, you will only take Progesterone, in a low dose, up to week 32 to keep your cervix long, strong and closed and to reduce the risk of a late miscarriage, or an early birth. In some cases, we recommend continuing with low dosages of Aspirin and low molecular Heparin to improve function of the placenta and reduce risk of late complications in the pregnancy such as preeclampsia.
We will also continue our dialogue with you, up to positive pregnancy test, ultrasound examination and onto live birth, advising and supporting you throughout this journey.
This is because we know that the pregnancy alone is not the desired result. The result is a baby in your arms.
Please contact us to arrange your online individual consultation with one of our doctors, this will allow them to talk personally with you about your medical history and then advise you on your ideal treatment plan for having a baby.
Some possible scenarios
Best luck Scenario (the shortest – takes 3 months)

Scenario 2 (takes 6 months)

Scenario 3 (takes 7 months)

Scenario 4 (takes 8 months)

Scenario 5 (takes 9 months)

There may be more scenarios that are less common: more IVF cycles and just one embryo transfer till pregnancy is achieved or just one IVF cycle and several embryo transfers until on-going pregnancy and baby. There may be even two hysteroscopies sometimes. But most importantly you should know that if we are moving logically step by step and do not lose time, it usually does not take longer than 9 months to achieve an on-going pregnancy.
We hope that our long-term experience of successful work with patients with the most difficult medical cases together with your perseverance and wish to reach the goal will help us achieve the birth of your healthy, strong and happy baby.
If you would like to discuss your situation and chances with us, please call or email us. We have time for you, and we will be happy to discuss any initial questions with you and agree on a time for an individual consultation with our doctor.
Q&A
- You recommend not more than two days of abstinence between the last ejaculation and sperm collection. What is the reason behind this?
- In the case of using frozen sperm samples for fertilization is there a possibility to perform regular IVF?
- Even though our clinic told us that the bad fertilization was mainly due to bad sperm (ICSI performed with a bad result – half of the eggs were fertilized abnormally with 3PN), it feels like my partner’s health was dismissed. We feel like it’s half of the equation for viable embryos, and that we need to go deeper into this subject.
- Is higher sperm motility always better? I.e. does MOT 50 has a higher success rate than MOT 20? Any difference depending on woman’s age? What do you use at your clinic?
- My question is about heat and sperm quality. How long before egg retrieval a man shouldn’t visit a sauna? For example, Is it OK for a man to go to a spa 1-2 months before? Or should he stay off heat for at least 74 days before leaving his sperm sample for treatment?
- It is clear that the quality of the egg plays a key role for success. So how can you help in improving the quality of the egg? How are your stimulation protocols different from other IVF clinics?
- How many simulations are “too much” (medically unsafe) and is it time to stop/change strategy?
- l have gained a significant amount of weight during my treatments (10 kg in 1 year) My question is if losing weight would increase my chances for a successful treatment in the future?
- Regarding Melatonin you recommended me to take, in Sweden we have to have a recipe to get it. And on the flyer that comes with it, it says that it’s not recommended to use it if one wants to get pregnant. Is it true? Do you have any brands that you can recommend?
- Is there a slow stimulation cycle and a normal one and how do you choose which one the woman should go through for extracting eggs? What are the criteria for choosing either? Does one of them have less chance of abnormal chromosomes in the eggs extracted and why if so?
- When pulling out the follicles, do you pull them all out? Both the ones which are small and the ones which are mature? Does it ever happen that a follicle is hidden and left behind?
- If only one or two eggs are collected in each IVF attempt, do you recommend culture to a blastocyst? I also have another question. Does your clinic offer in vitro maturation of eggs? 2 of my ivf cycles failed because the eggs were not mature when the clinic retrieved them.
- Hello, are the incubators you use time-lapse incubators? Do you/do you not recommend using them? Also, is the embryo culture media changed at Day 3, or is the same media used for both cleavage and blastocyst culture? Do you use EmbryoGen + BlastGen (culture media that has the addition of cytokine GM-CSF)? Do you find this helps (or not?)
- What is the «survival rate» for frozen embryos when thawed? Do you need to thaw more than one embryo to be sure when you prepare for an embryo transfer?
You recommend not more than two days of abstinence between the last ejaculation and sperm collection. What is the reason behind this?
The ejaculation can be even night before sperm collection, the 'fresher' the sample is the better. We are not after high concentration but after better motility and competence of the sperm which usually comes with less days of abstinence.
Dr. Anna Gusareva
Back to Index
In the case of using frozen sperm samples for fertilization is there a possibility to perform regular IVF?
With frozen samples we use ICSI almost always, except for donor sperm. The reason for that is because after freezing-thawing the motility usually drops twice so only samples which were "donor-like" at the time of freezing can reach the high parameters, suitable for IVF, after thawing and preparation.
Dr. Anna Gusareva
Back to Index
Even though our clinic told us that the bad fertilization was mainly due to bad sperm (ICSI performed with a bad result – half of the eggs were fertilized abnormally with 3PN), it feels like my partner’s health was dismissed. We feel like it’s half of the equation for viable embryos, and that we need to go deeper into this subject.
I understand your concern that usually less attention is paid to the male factor. I will explain why I think that the egg factor is the most important in your case as well as in many others. Poor fertilization results of your eggs after ICSI showed an interesting pattern in the pronuclear development — half of the eggs fertilized abnormally (3PN) which is a really rare case when ICSI is performed. During ICSI it is guaranteed that only one spermatozoid will be placed inside each egg, so presence of 3 pronuclei on the next day after ICSI indicates that two of these are from the egg, which means that egg was unable to complete meiosis properly — extrude the second polar body. It points toward egg problems with competence and cytoplasmic maturity.
To overcome that situation we propose to do more individualized stimulation aiming for more synchronous growth of the follicles and prolonging it to get more mature and competent eggs. We believe that following basic lifestyle recommendations (refrain from smoking and alcohol intake, healthy diet and physical activity) together with intake of the supplements (we will give you the individual list) will help to increase parameters of your sperm and bust its energetic potential.
Dr. Anna Gusareva
Back to Index
Is higher sperm motility always better? I.e. does MOT 50 has a higher success rate than MOT 20? Any difference depending on woman’s age? What do you use at your clinic?
No, if sperm motility is better it doesn't mean that the outcome of IVF will be better. Only in severe cases of asthenozoospermia with complete loss of sperm motility it could have an adverse effect on the fertilization rate. In all other cases, the origin and the quality of sperm doesn't matter in terms of the IVF result. Women's age, on the contrary, has a major effect on pregnancy + live birth rates and sperm motility doesn't add any difference.
Dr. Anna Gusareva
Back to Index
My question is about heat and sperm quality. How long before egg retrieval a man shouldn’t visit a sauna? For example, Is it OK for a man to go to a spa 1-2 months before? Or should he stay off heat for at least 74 days before leaving his sperm sample for treatment?
Yes, heat negatively affects sperm quality, especially the motility of sperm. So men should refrain from long lasting hot tubs and saunas during 2,5 months prior to sperm collection.
Dr. Anna Gusareva
Back to Index
It is clear that the quality of the egg plays a key role for success. So how can you help in improving the quality of the egg? How are your stimulation protocols different from other IVF clinics?
There are many stimulation protocols existent precisely because each woman is unique. So we are not inventing new ones but select the best one for your individual situation. The knowledge about your previous attempts and protocols/dosages/duration/follicular measurement/outcomes help us a lot. The more detailed information we have - the more tailored will be the approach to stimulation and overall strategy. It is immensely important for the competence of the eggs how they were ‘cooked’ — prepared for future fertilisation and development by the right stimulation and precise list of supplements you take for 2 months before the egg retrieval.
Dr. Anna Gusareva
Back to Index
How many simulations are “too much” (medically unsafe) and is it time to stop/change strategy?
It all depends on a woman's current general health and medical history. Also we calculate the probability of having a chromosomally normal embryo depending on the age, ovarian reserve and outcomes of previous attempts and discuss it with each patient. In each individual situation we assess the risks and benefits and decide if it is safe and useful or not to try again or should we use the alternative approach.
Dr. Anna Gusareva
Back to Index
l have gained a significant amount of weight during my treatments (10 kg in 1 year) My question is if losing weight would increase my chances for a successful treatment in the future?
The optimal BMI before the start of fertility treatment is below 30 kg/cm3. The risks of the high BMI include: lower pregnancy rate, increased miscarriage rate, pregnancy complications, as well as significant health risks for the baby. Switching to a healthier diet and adding some exercising to lower your BMI would increase your chances for success.
Dr. Anna Gusareva
Back to Index
Regarding Melatonin you recommended me to take, in Sweden we have to have a recipe to get it. And on the flyer that comes with it, it says that it’s not recommended to use it if one wants to get pregnant. Is it true? Do you have any brands that you can recommend?
Regarding the dosage of Melatonin we recommend is completely safe for the period of preparation for IVF or ET. After embryo transfer you will stop using it. It helps sleep well which is very important for hormone production and general wellbeing. You can use any brand. To learn more about the supplements we recommend and their role in the fertility process please watch our pre recorded webinar by Dr. Alena Egorova, you can request access to it here
Dr. Anna Gusareva
Back to Index
Is there a slow stimulation cycle and a normal one and how do you choose which one the woman should go through for extracting eggs? What are the criteria for choosing either? Does one of them have less chance of abnormal chromosomes in the eggs extracted and why if so?
Our doctors are choosing stimulation protocol individually, taking into consideration all previous attempts, current ovarian reserve, age and much more. During egg maturation its energy levels have to multiply hundred times. Older eggs have deficiency of energy resources and need even more time for maturation. Hence too short stimulations may be just not enough for the cytoplasm of the egg cell to mature.
Dr. Anna Gusareva
Back to Index
When pulling out the follicles, do you pull them all out? Both the ones which are small and the ones which are mature? Does it ever happen that a follicle is hidden and left behind?
During egg retrieval the doctor aspirates fluid from all follicles with the visual cavity, regardless of size. It happens that some of the eggs we get from such follicles are immature but in some cases mature eggs could come from small follicles and vice versa. On ultrasound all follicles with cavity are usually seen quite clearly, so doctor wouldn't miss them. But in some rare cases the anatomy of ovaries could be quite unusual and follicles could be hard to get by transvaginal access.
Dr. Anna Gusareva
Back to Index
If only one or two eggs are collected in each IVF attempt, do you recommend culture to a blastocyst? I also have another question. Does your clinic offer in vitro maturation of eggs? 2 of my ivf cycles failed because the eggs were not mature when the clinic retrieved them.
Yes, we always culture embryos to the blastocyst stage, disregarding the quantity of the eggs. We are confident in our culture conditions and believe it is better to transfer a viable embryo. So, if the embryo doesn’t look viable we recommend not to transfer it and save a patient from this hard 2 week wait. We do not practice IVM because it is still an experimental technique and has a lot of limitations. But we have many patients with previously immature eggs only, who got mature eggs with the help of our doctors’ individualized stimulation. Do not give up your eggs before you try our individual stimulation.
Dr. Anna Gusareva
Back to Index
Hello, are the incubators you use time-lapse incubators? Do you/do you not recommend using them? Also, is the embryo culture media changed at Day 3, or is the same media used for both cleavage and blastocyst culture? Do you use EmbryoGen + BlastGen (culture media that has the addition of cytokine GM-CSF)? Do you find this helps (or not?)
Great questions! I see you are a pro! We do not have time-lapse incubators in the lab. There is no hard evidence that culturing embryos in these incubators will make a significant difference in terms of success rates. They provide good conditions for embryos because their culture is not interrupted by openings but the usefulness of time-lapse itself is debated by the scientific community. We use the same principle of uninterrupted culture in the same drop of media from Day 1 till Day 6, taking embryos out of the incubator only 3 times for a very brief period (on days 3,5 and 6).
We are using benchtop multi gas incubators which restore the initial conditions for the embryos very quickly, so these observations don't harm them at all and the information we get is enough. So basically, time-lapse incubators for now are more of marketing than of real usefulness. Embryo-Gen and Blast-Gen can be useful for a very specific group of patients and we are considering trying it but have no own experience on them. There is no hard evidence they will help the unselected patient’s population, unfortunately.
Dr. Anna Gusareva
Back to Index
What is the «survival rate» for frozen embryos when thawed? Do you need to thaw more than one embryo to be sure when you prepare for an embryo transfer?
Survival rate for the vitrified blastocysts in our clinic is around 95%. So most of the time we thaw only one blastocyst with the best score available at least 2 hours before transfer. In rare cases, if the embryo doesn't look well after thawing, we have enough time to thaw one more.
Dr. Anna Gusareva
Back to Index