PGT-A, or preimplantation genetic testing for aneuploidies, is a comprehensive screening performed on embryos before transfer. This test reveals the set and structure of chromosomes (bearing genetic material) in each tested embryo.
Normally, embryos have 23 pairs of chromosomes (euploid embryos). But nearly half of the embryos will have abnormal chromosome set (aneuploid embryos). When an extra, or missing chromosome, is found in the embryo it is less likely to implant. If the implantation did take place, then, unfortunately, there is a high probability that a pregnancy with such an embryo will end in a spontaneous loss. In some cases, such a pregnancy can still develop to full term, but a baby with a genetic condition will be born (e.g. Down syndrome — an extra chromosome 21).
PGT-A tests the set of chromosomes in DNA taken from embryos. Embryos with an abnormal set of chromosomes will not lead to a healthy live birth, hence they are excluded from use. Embryos with a normal set of chromosomes would be used for the embryo transfer.
| PGT-A does not make the embryos better, PGT-A shows which embryos have a normal set of chromosomes from those available |
Chromosomal screening helps to select the best embryo for transfer - so your chances of getting pregnant are higher, and miscarriage rates are lower, after the transfer of not only a good-looking, but also euploid embryo. On Figure 1 you can see an example of two excellent morphology embryos with corresponding PGT-A results: a — abnormal (missing chromosome 22), b — normal. Despite the seeming similarity, these embryos have different prospects: the transfer of an a-embryo will not result in a successful pregnancy; the transfer of a b-embryo will result in an ongoing pregnancy and live birth with a 49% chance.
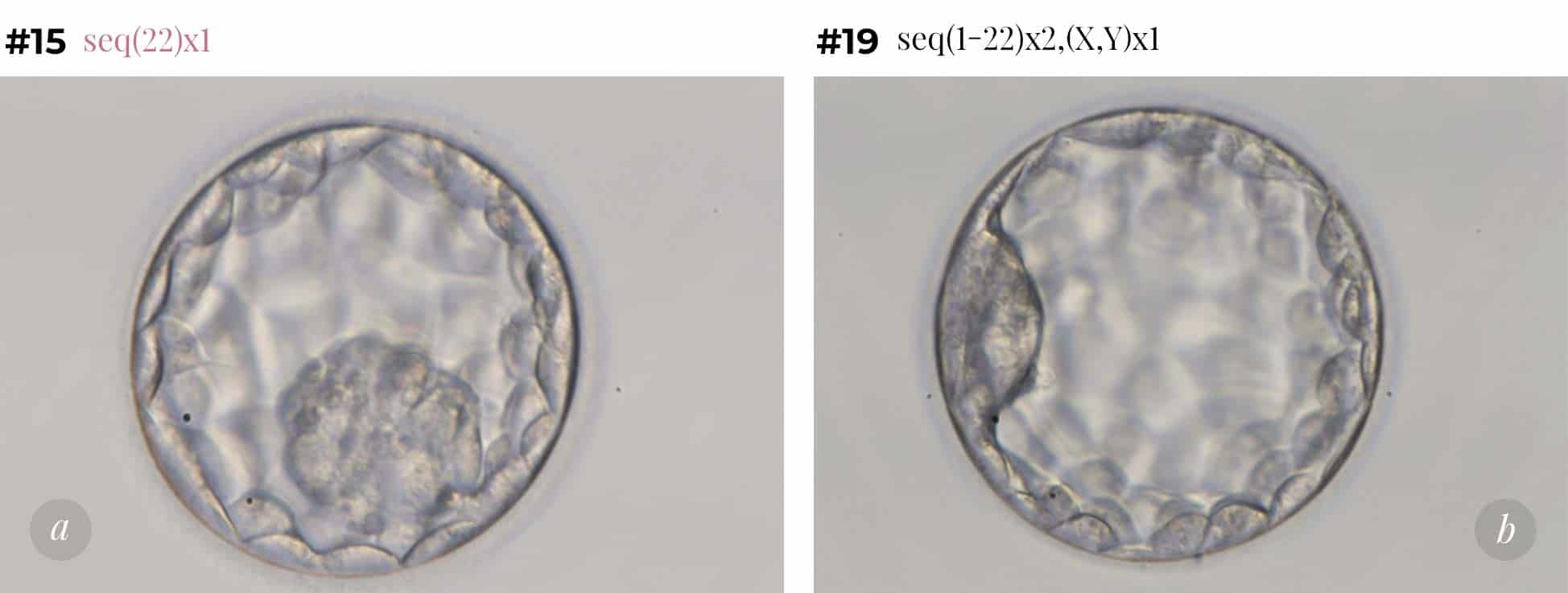 Fig.1 Best quality blastocysts, from a patient of 39 years old, showing different PGT-A results:
Fig.1 Best quality blastocysts, from a patient of 39 years old, showing different PGT-A results:
a) abnormal (missing chromosome 22);
b) normal.
What are the goals of PGT-A?
- To increase pregnancy rates
- To reduce miscarriage rates
- To increase live birth rates per embryo transfer
- To shorten the time to pregnancy (reduce the number of embryo transfers required to create a pregnancy)
Have questions?
What are the indications for PGT-A?
To get the DNA from the embryo we need to biopsy it. Embryo biopsy, despite its safety, is an invasive procedure. It is another additional step in IVF, so needs solid indication of the benefits before being carried out.
But there are, in several patient groups, unquestionable benefits for using PGT-A.
Indications for PGT-A:
- Advanced maternal age;
- Recurrent Early Pregnancy Loss;
- Chromosomal rearrangements in karyotype of one of patients.
Advanced Maternal Age
It is well-documented that the chromosomally abnormal status of an embryo is contributed mainly by the egg (more than 90%). Maternal age is crucial for the genetic constitution of the egg and hence of the embryo, as the embryo derives from the egg.
PGT-A is a very helpful method for women above 35 to shorten time to pregnancy.
What proportion of embryos at blastocyst stage are expected to have a normal set of chromosomes?
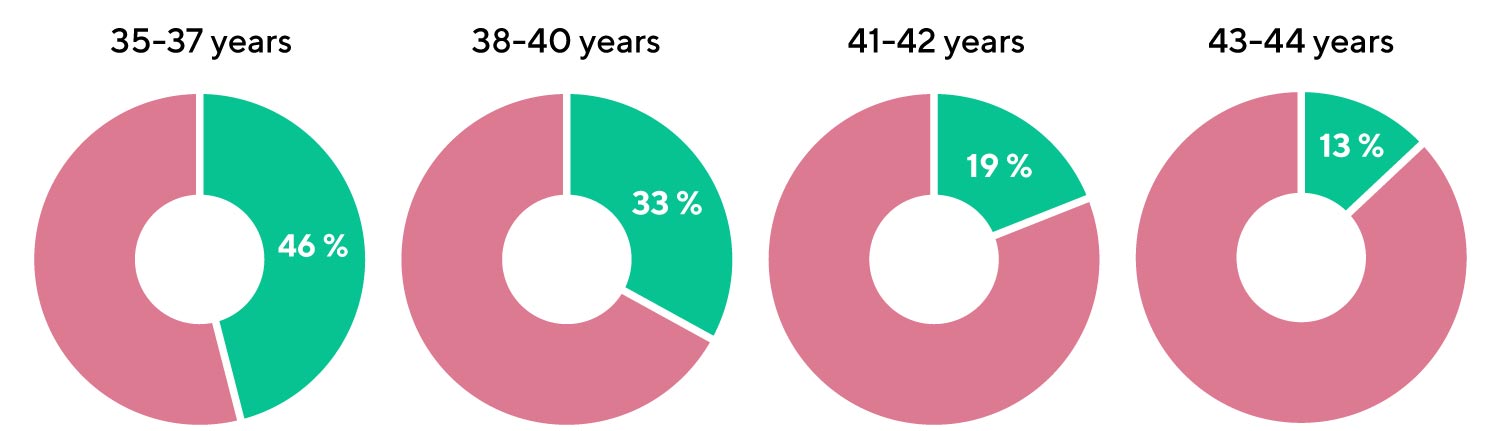
[Munne, S. et al. (2015). Blastocysts needed to transfer at least one euploid embryo: data from 10,852 pre-implantation genetic screening (PGS) cycles. Fertility and Sterility, Volume 104, Issue 3, e13 - e14]
- Every second blastocyst is expected to have a normal set of chromosomes in the age group 35-37;
- Only one in 8 blastocysts is expected to have a normal set of chromosomes by the age of 43.
According to various extensive studies, women aged 35 and older, have a significant increase in live birth rates per embryo transferred after PGT-A, in comparison to control. Also, in many cases (spontaneous pregnancy losses, IVF failures) PGT-A can help increase IVF success for women under the age of 35 years old.
Diagram 1. STAR Trial Compared with SART (National Summary report USA (2014-2017). Pregnancy outcomes
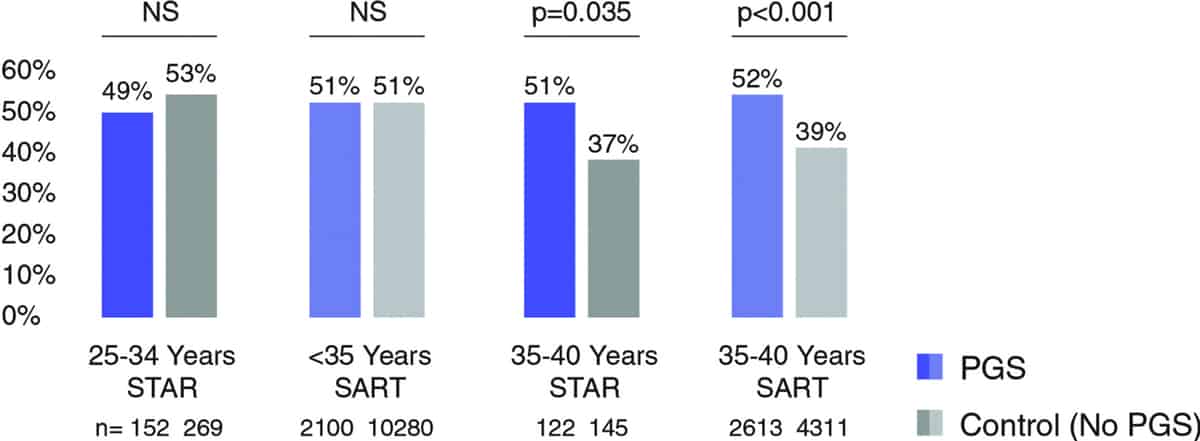
STAR — 20-week ongoing pregnancy rate per transfer, note that all 20-week ongoing pregnancies resulted in a live birth
SART — Live birth rate per eSET
PGT-A does not increase success rates in egg donation or double donation cycles, since eggs from younger women are used. PGT-A just makes the cost of success higher in egg donation and double donation cycles.
Recurrent Early Pregnancy Loss
Multiple, unsuccessful, IVF attempts and miscarriages are very upsetting and frustrating for patients. If the cause of the previous failures was aneuploid embryos, these patients will also then benefit from PGT-A.
Chromosomal rearrangements in karyotype of one of patients
If a person carries balanced chromosomal rearrangements — their embryos are at greater risk of aneuploidy. These cases are rare, but the only effective and safe treatment for it is IVF with PGT-A.
How is PGT-A done?
The only way to perform PGT-A is during IVF cycle.
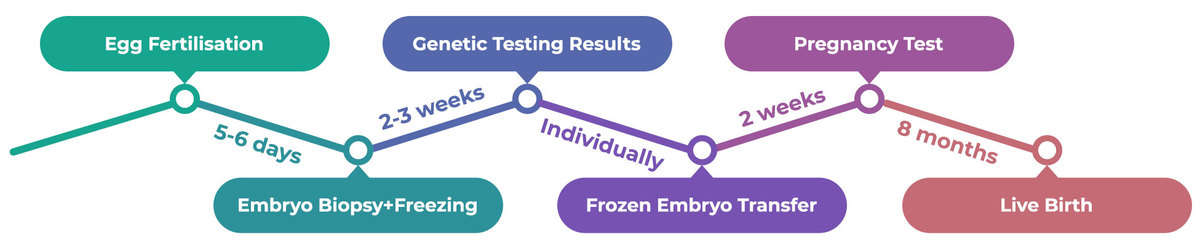
- Egg Fertilization
After fertilization the embryos grow in the lab for 5-6 days and become blastocysts. During that time, natural selection is in action, so on average only half of the fertilized eggs reach blastocyst stage. Those that stopped their development are believed to be genetically incompetent. - Embryo Biopsy + Freezing
Blastocysts with good morphology are biopsied on Days 5-6. During the biopsy an embryologist takes 3-7 cells from the outer part of the blastocyst (trophectoderm, TE). The inner cell mass (ICM) of the blastocyst remains intact, so there is no harm to the future baby. Biopsies from each blastocyst are marked and sent to the genetics lab for analysis. Then the blastocysts are frozen and stored individually.
 Fig. 2. Blastocyst biopsy. ICM — inner cell mass (future baby), TE — trophectoderm (future embryonic placenta)
Fig. 2. Blastocyst biopsy. ICM — inner cell mass (future baby), TE — trophectoderm (future embryonic placenta) - Genetic Testing Results
There are several methods for PGT-A, the most modern and reliable is next generation sequencing (NGS). It takes around two weeks to gain the results from the genetic lab for each embryo. - Frozen Embryo Transfer
When the genetic results are ready, and at least one euploid embryo is available based on PGT-A result, the preparation of endometrium for embryo transfer begins. On the day of transfer an embryologist thaws the chosen embryo and prepares it for transfer.
Have questions?
How to interpret the results of PGT-A?
The sensitivity (no false negatives) and specificity (no false positives) of NGS method of PGT-A are around 95-98%, as confirmed by various authors. It means that you can trust the results, but also that no diagnostic method can give 100% accuracy.
Embryos are highly dynamic structures, embryonic cells divide very actively, so genetic errors in these divisions can occur. This leads to a mosaicism of the embryo — different cells in the embryo may have a different set of chromosomes. But the biopsy only takes out 3-7 cells of the blastocyst, so the question is – ‘are these cells representative of the rest of the embryo’? For now, the answer is ‘YES’ in most cases, these cells are concordant (representative) of the others.
Results for each embryo will be given by a simple definition — ‘recommended for transfer’, ‘not recommended for transfer’, or ‘recommended upon signing the consent form’. But, what does this later definition usually mean? In most cases those embryos are considered mosaic or bearing some light form of abnormalities. Mosaicism in the fetus and newborn baby is a much rarer event than in the embryo, so there must be some mechanism for the elimination of abnormal cells throughout pregnancy.
If you receive a PGT-A result of some embryos being considered as mosaic, it is better to plan an appointment with your doctor to assess the possible risks and benefits of transferring a mosaic embryo. If euploid embryos are also available for transfer, then preferably these should be transferred instead.
Have questions? Book an online consultation with one of our expert doctors to discuss your questions and your individual medical situation.
Q&A
- My doctor in the Netherlands told me that US studies showed that sometimes chromosome abnormalities can fix themselves in early stages of development. Which means that genetic testing could potentially rule out embryos that could lead to pregnancies. Is it true?
- In what genetic lab the PGT-A will be performed? Is it the Igenomix Laboratory in Spain? Will you perform the regular PGT-A or the new one from Igenomix called “Embrace”, where only the culture environment is analysed?
- I wonder if you can see in his sperm if there’s any defective genes coming from the sperm, for example ADHD or Asperger’s syndrome? I have read that the autism spectrum increases in the offspring the older the father is.
My doctor in the Netherlands told me that US studies showed that sometimes chromosome abnormalities can fix themselves in early stages of development. Which means that genetic testing could potentially rule out embryos that could lead to pregnancies. Is it true?
It is true, embryos are dynamic structures and can change all the way. But the probability of PGT-A testing being wrong is pretty low, below 1-2%. But the benefit of testing is obvious in the older group of patients - you have much less chance that the pregnancy will not happen or that it will stop, leading to possible complications for the uterus and jeopardising your future chances for a baby, not to mention the psychological burden of that. Here I will be on the mother's side, even if it means not giving a chance for some potential babies. But this is a highly disputable topic nowadays, you can find arguments both pro and contra.
Dr. Anna Gusareva
Back to Index
In what genetic lab the PGT-A will be performed? Is it the Igenomix Laboratory in Spain? Will you perform the regular PGT-A or the new one from Igenomix called “Embrace”, where only the culture environment is analysed?
Usually PGT-A by NGS method is conducted in the Igenomix laboratory in Russia or Genetico lab also in Russia. We use these providers for a long period of time and are quite satisfied with the results. Blastocysts will be biopsied and frozen subsequently, the result we expect in 2 weeks. "Normal" PGT-A is the most reliable at the moment. Unfortunately Embrace results (testing of the spent culture media) are not so concordant with the real molecular karyotype of the embryo for now. We hope it will become more reliable in future but the current reality leaves us with only choice - if we need THE answer, trophectoderm biopsy + NGS is the best available approach. Our embryologists are very skilled in performing biopsy, we do it a lot, so you shouldn't worry about us harming the embryo in any way or diminishing its potential.
Dr. Anna Gusareva
Back to Index
I wonder if you can see in his sperm if there’s any defective genes coming from the sperm, for example ADHD or Asperger’s syndrome? I have read that the autism spectrum increases in the offspring the older the father is.
Unfortunately current level of science doesn’t give an opportunity to check spermatozoa for mutations before the fertilization. The checking could only be done on an embryo but only in such cases when we know that potential parents are known carriers of certain gene mutations. To check mutations in general is impossible for now.
Dr. Anna Gusareva
Back to Index